The extent and impact of inaccurate NHS patient records

Accurate patient medical records are crucial to delivering effective and efficient care. Healthcare professionals rely on medical records to support them in providing patients with the treatment they need.
Most of us will have a lifelong NHS GP record, as well as any individual records held by other NHS services about our healthcare, such as hospitals, dentists and even pharmacies, as they start to deliver some consultations.
The NHS is investing resources and funding into making patient records paperless and improving patient information sharing between services.
However, coroners have repeatedly issued warnings about inadequate information sharing in the NHS, with some patients dying because clinicians could not access important details about their needs. But is the information in patient records correct in the first place?
What have people told us about their NHS patient records?
Earlier this year, we reviewed our recent feedback on patient records and found people reporting alarming issues with medical records.
To estimate the extent to which inaccurate records are widespread, we commissioned BMG Research to conduct a nationally representative survey of 1,800 adults between 24 and 27 March 2025.
Concerningly, we found that nearly one in four (23%) adults have noticed inaccuracies or missing details in their medical records before. It is unclear how many of these individuals have since been able to correct their records, though patient feedback indicates that correcting records can be a long and/or difficult process.
What inaccuracies have people found in their NHS records?
We asked the people affected what inaccuracies they had noticed. In most cases, people said they had noticed missing information, though some said their records contained incorrect information.
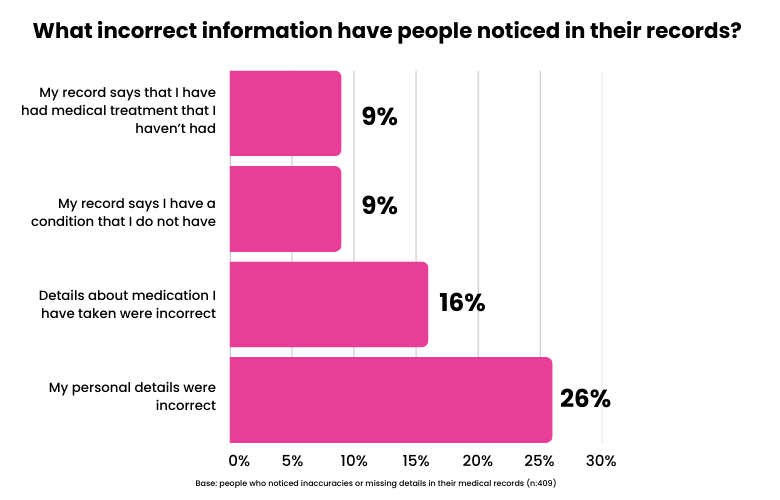
Incorrect information on NHS patient records
Incorrect information can cause both inconveniences and represent a clinical risk to individuals. For example, the most common issue is inaccurate personal details, such as name or date of birth.
A quarter (26%) of those who have noticed inaccuracies in their records said their personal details were wrong. Many elements of NHS care involve individual staff members verbally carrying out ‘positive identification checks’ with patients, using date of birth information, especially if the person’s NHS number is unavailable at the time. A national safety body has found that misidentification can have serious consequences, such as the wrong surgery being carried out.
Other errors include inaccurate records of medications, diagnoses or treatments. Over one in seven (16%) of those who reported an inaccurate record said that this related to inaccurate information about what medication they had taken.
Just under one in ten (9%) of those who have noticed inaccuracies said there is a record of a condition they do not have, and the same proportion (9%) say their records detail medical treatment they have not had. We heard from a few people describing this experience.
“According to NHS records, I have had 2 full and one partial hysterectomies. I also have 5 flu jabs recorded in the space for 4 days when I hadn’t even had one.”
Story shared with Healthwatch England.
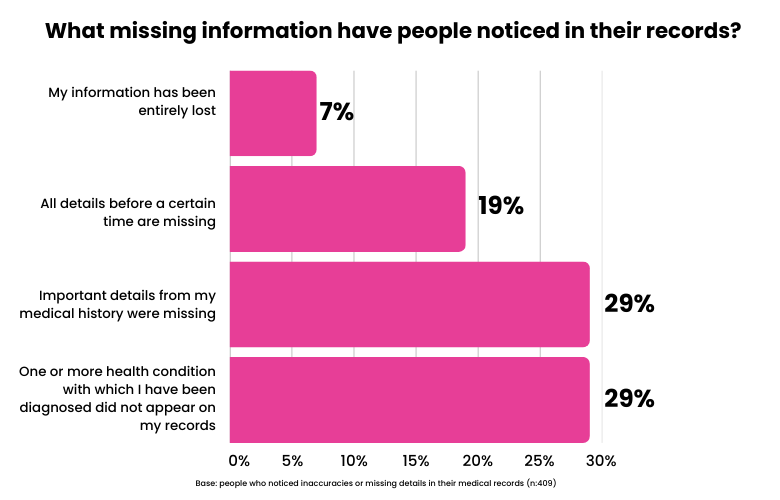
Missing information
When it comes to missing information, 29% of those who have noticed inaccuracies in their records said that one or more diagnosed health conditions are not on their medical record. The same proportion (29%) said important information from their medical history is missing, such as periods of serious ill health or time spent in hospital.
"I have diabetes, IBS, diverticulitis, arthritis, high blood pressure, high cholesterol, sacroiliac problems and only a few of these appear on my records.'"
Story shared with Healthwatch England.
For some, this is not just a case of minor errors here and there: nearly one in five (19%) of those who have noticed inaccuracies say all details before a certain date are missing in their record.
When considering these figures for missing information, we should note that the records you can see on the NHS App are not your full records. Rather it is a summary of your GP record, usually dating back only to November 2023, when technology changed.
Information added to the NHS App from other sources, such as hospital letters and test results, currently varies, and people may have to go to each service to request a copy of their full records. This represents an issue, demonstrating the need for clear communication to help people understand how their records work.
What is the impact of inaccurate NHS patient records?
Accurate information about patients in the NHS is essential. Inaccurate information can, in extreme cases, result in serious harm or even death.
Our findings underline how impactful inaccurate records can be, with fewer than one in five (17%) of those who have noticed inaccuracies in their records saying it has not impacted them.
The most common consequence is the inconvenience of filling in the missing information for medical professionals during appointments. Over one in four (26%) of those who have noticed inaccuracies say they must repeat their patient history, which can be frustrating.
We heard that this frustration is exacerbated by healthcare staff who are not always receptive to patients’ descriptions of their medical history.
"Exhausting and very annoying for me to have to start everything over when GPs can tend to be sceptical to patients’ descriptions of diagnoses and tests that are not on their records."
Story shared with Healthwatch England.
Unfortunately, experiences like this are not an isolated incident. One in five (20%) of those who have noticed inaccuracies in their records say they have struggled to convince healthcare staff about something from their medical history because it does not appear in their records.
Sometimes, inaccurate patient records may lead to poor or incorrect treatment and care. We have heard from people who have received unsatisfactory care based on the inaccurate contents of their medical records.
"Been in three care homes; each quote from out of date/no longer relevant/inaccurate GP records on which to base my care. Try to put them right but they say “we can only put down what your GP records say”. Have even shown them hospital letters, but no notice taken."
Story shared with Healthwatch England.
Our polling underlines the risk posed by inaccurate medical records. Over one in eight (13%) of those who have noticed inaccuracies in their records said they had not received an important test or treatment that they would have if the information had been correct.
A similar number of people (12%) said they had been refused treatment because of inaccurate or missing information. Concerningly, 10% said they have been given incorrect or inappropriate medication, and 9% said they have received potentially unsafe care or treatment.
The impact of inaccurate medical records extends beyond health care. The information contained in medical records may be used in legal matters, insurance, benefit claims, and other areas.
Over one in eight (13%) of people who have noticed inaccuracies in their record said it has negatively impacted something outside of healthcare. We heard from someone who encountered issues getting their Personal Independent Payment (PIP) because of missing information in their record.
"A large chunk of my medical records have gone missing. I only found out because I wanted to apply for PIP again as I was turned down a few years before because of lack of evidence. I've gone through all the official routes but no one seems to be able to give me an answer."
Story shared with Healthwatch England
Finally, we learned how inaccurate records create inefficiencies that frustrate patients and waste NHS resources. People told us about repeated tests or consultations and invitations for tests or consultations about something irrelevant to them.
"The amount of times I am sent for the SAME appointments like physio therapy when ALL my PTs have told me they CANNOT help with my spinal degeneration yet with every new doctor I see they send me BACK for the same treatments at PTs."
Story shared with Healthwatch England.
Adding to the potential negative impact on care and treatment, we also heard stories raising concerns about potential confidentiality breaches. Some patients told us that they discovered that their records contained information about someone else. In some cases, patients have realised the information is about a family member with whom they share a name and thus can identify the other individual involved. This raises serious GDPR and privacy issues.
How does inaccurate information get into medical records?
People told us about two primary ways they believe inaccurate information about them got into their records.
The first is inaccurate notetaking by staff. We heard concerns from people that staff do not always take sufficiently detailed and accurate notes, which can lead to important information not going into records or inaccurate information being recorded. Several people told us how difficult it is to change a record once the information is in it, so even once the patient is aware of the inaccurate information, it can stay on their record for a long time.
The other way is the lack of integration between different healthcare services. We heard multiple stories of records getting ‘lost’ between services. GP Practices were a recurring theme in the stories we heard, with people identifying the point at which they moved GP Practice as when their record became incomplete.
Often, records from before a certain time seem to get ‘lost’, something shown in our polling where 19% of those who have noticed inaccuracies in their record said all details before a certain time are missing. Worryingly, 7% said that their information had been lost entirely.
In practice, this information is not ‘lost’ but is not correctly communicated from service to service, resulting in services having different records. There is no single NHS record for each person covering every service.
Further research needed
More younger people say they are aware of inaccuracies on their record than older people, with a third (33%) of people between 18 and 24 saying so. This compares to fewer than one in five (17%) people over 65.
We cannot say from our research whether more younger people’s records have inaccuracies or if younger people are simply more likely to have become aware of inaccuracies. This is something that warrants further investigation.
What needs to happen?
Our research suggests that many people have inaccuracies in their medical records and that, for many of these people, this negatively impacts their healthcare and beyond. Moreover, our research only highlights the people who have noticed inaccuracies in their records. We cannot say how many more people may have inaccurate records but do not know about it.
It should be noted that inaccuracies are often due to human error. This is understandable when stretched and hardworking staff are under significant pressure. Ultimately, improving the working culture and conditions in services will help address some of the issues we have identified.
However, three clear actions could also improve the situation.
- Better record keeping. These stories and figures highlight the urgent need for improved record-keeping practices. This could be achieved by promoting relevant guidance and regulations by professional regulators, as well as better interoperability to ensure records are shared effectively. The government’s ambition to have a single patient record should help address this.
- Promotion of people’s rights to get records amended. People's right to do this needs to be clearer, along with the legal reasons why services may still have to retain a record of contested information. It is also important to make more people aware that they can complain to the NHS or the Information Commissioner’s Office.
- Clearer guidance for patients about how to change incorrect records. People told us how difficult it is to amend or remove inaccurate information in their records.
"ALL medical practitioners should be responsible for accurately recording notes, patient's descriptions of symptoms, etc., and be mindful of the potential consequences to the patient of inaccurate recording in patient records and correspondence, etc., being fully aware that any discrepancies can have serious adverse repercussions for the patient, not only in terms of their health, but also legal, insurance, benefits, employment, etc; in other words, what the medical professional records is what is ultimately 'believed' by their peers."
Story shared with Healthwatch England.
Last October, the Government announced it would create a ‘single patient record’ through the NHS App, which would summarise patient health information, test results, and letters in one place. This will, the Government said, ‘put patients in control of their own medical history, meaning they do not have to repeat it at every appointment, and that staff have the full picture of patients’ health’.
New laws to make patient health records available across all NHS trusts, GP surgeries, and ambulance services in England are expected to support this, speeding up patient care, reducing repeat medical tests and minimising medication errors.
We will share our new findings with the Government to help inform its plans.
About the poll
BMG Research interviewed a representative sample of 1,800 adults in England online between 24-27 March 2025. BMG Research is a member of the British Polling Council and abides by its rules.
Want to find out about your patient records?
Our advice article can help you understand where are your records kept now, how can you view them, and what do you do if you find mistakes in them.



